An endoscopy is a test that lets your doctors look inside your body. They use an endoscope to do this. An endoscope is a long, thin, flexible tube with a tiny light and camera at one end.
The camera sends images for your doctors to look at on a screen.
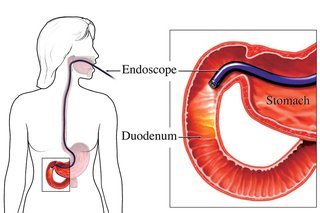
Your doctor passes an endoscope into your body through a natural opening, such as your mouth.
They can also insert it through a small cut (incision) in your skin if you are having keyhole surgery.
When an endoscopy is used
An endoscopy can:
- investigate symptoms, such as blood in your poo
- help treat a condition
An endoscopy can be used as part of the bowel screening process. For example, if you did a bowel screening home test and your result was 'not normal'. You may be asked to go for an endoscopy.
An endoscope can also remove a small sample of tissue for analysis in a laboratory. This is known as a biopsy.
Your consultant will tell you how long it takes to get your test results.
Investigating symptoms
You may need an endoscopy if you have:
- difficulty swallowing (dysphagia)
- abdominal (tummy) pain that does not go away
- chest pain that is not caused by heart-related conditions
- nausea and vomiting that does not go away
- weight loss that cannot be explained
- vomiting blood
- diarrhoea that does not go away
- blood in your poo
Types of endoscopy
There are different types of endoscopy. The test you have will depend on your symptoms and the part of your body affected.
Types of endoscopy include:
- gastroscopy - for your oesophagus (food pipe), stomach or first part of your small intestine (duodenum)
- colonoscopy - for your bowel
- bronchoscopy - for your airways, if you have a cough that does not go away or you're coughing up blood
- hysteroscopy - for your womb (uterus) if you have unusual vaginal bleeding or repeated miscarriages
- cystoscopy - for your bladder if you have urinary incontinence or blood in your urine
- endoscopic ultrasound - creates images of organs, such as your pancreas, and takes tissue samples
- arthroscopy - checks and treats problems with your joints
Treating conditions
Your surgeon can use an endoscope to help treat certain conditions.
Therapeutic endoscopy
Therapeutic endoscopy is where your surgeon attaches small surgical instruments to an endoscope to do an operation.
For example, an endoscope may be used to:
- remove gallstones, bladder stones or kidney stones - the procedure to remove gallstones is known as an endoscopic retrograde cholangiopancreatography
- repair damage inside joints (arthroscopy)
- repair a bleeding stomach ulcer
- put a stent in an area that is narrowed or blocked
- tie and seal the fallopian tubes (female sterilisation)
- remove small tumours from the lungs or digestive system
- remove fibroids - non-cancerous growths in the womb
Keyhole surgery (laparoscopy)
A laparoscope is a type of endoscope surgeons use for keyhole surgery (laparoscopy).
During keyhole surgery, the surgeon makes a few small incisions (cuts). This is instead of one large incision (open surgery).
Some of the advantages of keyhole surgery include:
- a shorter hospital stay and faster recovery time
- less pain and bleeding after the operation
- reduced scarring
Keyhole surgery is often used to repair hernias.
It is also used to remove:
- your appendix if you have appendicitis
- your gallbladder - to treat gallstones
- part of your intestine - to treat conditions such as Crohn's disease or diverticulitis
- your womb (hysterectomy)
- part or all of an organ affected by cancer
A laparoscope is also often used to help diagnose many different conditions.
What happens during an endoscopy
An endoscopy is usually done in an endoscopy unit in a hospital.
Before having an endoscopy
Depending on the type of endoscopy, you may be asked to fast (not eat or drink) for some hours before the procedure.
You may be given a laxative to help clear your bowels if you are having:
- a colonoscopy to examine the large intestine
- a sigmoidoscopy to examine the rectum and lower part of your bowel
Sometimes you are prescribed antibiotics to reduce the risk of an infection.
If you're taking a medicine to thin your blood, such as warfarin or clopidogrel, you may be asked to stop taking it for a few days before the endoscopy. This is to reduce the risk of bleeding.
Take any other medicines as normal, unless your GP or specialist tells you not to.
The endoscopy procedure
An endoscopy is not usually painful. Most people have mild discomfort after the procedure, like indigestion or a sore throat.
The procedure is usually carried out while you're awake. You may be given a local anaesthetic to numb a specific area of your body. For example, a spray or lozenge to numb your throat.
You may also be offered a sedative to help you relax.
The endoscope will be carefully inserted into your body. Where it's inserted will depend on the part of your body being examined.
For example, it may be inserted into your:
- throat
- bottom (anus)
- urethra - the tube that carries pee out of your body
If you're having keyhole surgery (laparoscopy), the endoscope will be inserted into a small cut (incision) your surgeon makes in your skin.
An endoscopy takes between 15 and 60 minutes. You usually have it as an outpatient, so you will not have to stay in hospital overnight.
Wireless capsule endoscopy
A wireless capsule endoscopy is a procedure that uses a tiny wireless camera to take pictures inside your stomach and digestive system.
The camera sits inside a capsule about the size of a large pill. You swallow the capsule and the camera collects images.
It's often used to investigate internal bleeding in the digestive system when there's no obvious cause.
The capsule leaves your body naturally when you poo.
There are some risks of complications with wireless capsule endoscopy.
It can:
- be difficult to swallow
- be difficult to pass naturally
- get caught in the narrow areas of your bowel, causing a blockage
After an endoscopy
After an endoscopy, you'll probably need to rest for about 1 hour until the effects of the local anaesthetic have worn off.
If you had a sedative, you will need to get a lift home.
If you've had a cystoscopy to examine your bladder, you may have blood in your urine for 24 hours afterwards. This should settle, but contact your GP if it continues.
Risks of an endoscopy
An endoscopy is a safe procedure. The risk of complications is very low.
Possible complications include:
- an infection in the area the endoscope was inserted - you may need to take antibiotics
- piercing or tearing (perforation) of tissue or an organ - you may need surgery to repair any damage
- excessive bleeding - you may need a blood transfusion
Sedation
Sedation is usually given by injection. It is usually safe, but sometimes it can cause complications.
These include:
- feeling sick (nausea) or getting sick
- a burning sensation at the injection site
- saliva or small pieces of food falling into the lungs, causing an infection - this is rare
- an irregular heartbeat
- low blood pressure
- breathing difficulties
Non-urgent advice: Speak to your GP if
- you have signs of an infection where the endoscope was inserted, such as:
- redness, pain or swelling
- a discharge of fluids or pus
- a high temperature of 38 degrees Celsius or above
Emergency action required: Contact your GP or visit your nearest emergency department (ED) immediately if you:
- have black or very dark-coloured poo
- are short of breath
- have severe tummy (abdominal) pain that does not go away
- are vomiting blood
- have chest pain
Content supplied by the NHS and adapted for Ireland by the HSE
