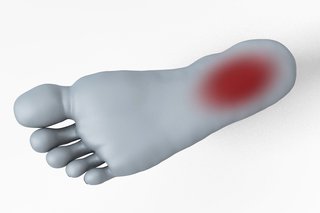
Plantar fasciitis is where you have pain on the bottom of your foot, around your heel and arch. You can usually ease the pain yourself, but contact your GP if the pain does not improve within 2 weeks.
Check if you have plantar fasciitis
It's more likely to be plantar fasciitis if:
- the pain is much worse when you start walking after sleeping or resting
- the pain feels better during exercise, but returns after resting
- it's difficult to raise your toes off the floor
Common causes of plantar fasciitis
Plantar fasciitis is caused by straining the part of your foot that connects your heel bone to your toes (plantar fascia).
It is not always clear why this happens.
You may be more likely to get plantar fasciitis if you:
- recently started exercising on hard surfaces
- exercise with a tight calf or heel
- overstretch the sole of your foot during exercise
- recently started doing a lot more walking, running or standing up
- wear shoes with poor cushioning or support
- are very overweight
Easing plantar fasciitis at home
If you contact your GP, they'll usually suggest you try these things:
Do
-
rest and raise your foot on a stool when you can
-
put an ice pack (or bag of frozen peas) in a towel on the painful area for up to 20 minutes every 2 to 3 hours
-
wear wide comfortable shoes with a low heel and soft sole
-
use soft insoles or heel pads in your shoes
-
regular gentle stretching exercises
-
exercises that do not put pressure on your feet, such as swimming
-
take paracetamol
Don't
-
do not take ibuprofen for the first 48 hours
-
do not walk or stand for long periods
-
do not wear high heels or tight pointy shoes
-
do not wear flip-flops or backless slippers
-
do not walk barefoot on hard surfaces
You can ask a pharmacist about:
- the best painkiller to take
- insoles and pads for your shoes
- if you need to see a GP
Non-urgent advice: Contact your GP if:
- the pain is severe or stopping you doing normal activities
- the pain is getting worse or keeps coming back
- the pain has not improved after treating it yourself for 2 weeks
- you have any tingling or loss of feeling in your foot
- you have diabetes – foot problems can be more serious if you have diabetes
What we mean by severe pain
Severe pain:
- always there and so bad it's hard to think or talk
- you cannot sleep
- it's very hard to move, get out of bed, go to the bathroom, wash or dress
- you cannot work due to the pain
Moderate pain:
- always there
- makes it hard to concentrate or sleep
- you can manage to get up, wash or dress
Mild pain:
- comes and goes
- is annoying but does not stop you from doing things like going to work
Treatment for plantar fasciitis from a foot specialist
Your GP might refer you to a physiotherapist for exercises or to see a foot specialist (podiatrist). They can recommend things like insoles and the right shoes to wear.
Content supplied by the NHS and adapted for Ireland by the HSE
