Shortness of breath is a common symptom of COVID-19. Some people describe it as feeling ‘puffed’, ‘breathless’ or ‘winded’.
The feeling of shortness of breath may continue for a while after your illness. This is a normal part of the recovery process.
Everyday activities can make you feel short of breath, for example:
- getting dressed
- walking to the bathroom
- climbing stairs
- doing jobs around the house
When you learn to control your breathing, your stamina will improve. You will then be able to do more before feeling short of breath.
Things to try when you feel short of breath
Feeling short of breath can make you feel tense, panicked or anxious. This can then make your shortness of breath worse.
When you feel shortness of breath, try to:
- stop speaking and moving
- give yourself time to recover your breath
- relax or distract yourself by focusing on a picture or a view from the window
- find a position to help your breathing
- do exercises to control your breathing
Managing shortness of breath is about controlling your breathing. You can do this no matter how fast or shallow your breath.
Positions to help your breathing
When we feel short of breath, we often tense the muscles in our neck and shoulders. This can make the feeling of shortness of breath worse.
Relaxing the muscles in your neck and shoulders can help. There are different positions you can try to relax these muscles and make it easier for you to breathe.
Sitting leaning forward
Sit leaning forward resting your elbows on your knees or the arms of the chair.

Sitting leaning forward at a table
Sit leaning forward with your elbows resting on a table. You could put some pillows or cushions on the table for comfort.

Standing leaning forward
Lean forwards resting your elbows on a chair, a wall or a railing. You could use a walking stick or a frame if you use one for walking.
Breathing techniques can be taught to you by your nurse or physiotherapist.

How to control your breathing
Relaxed tummy breathing
This breathing technique can help if you are breathless after doing any activity. It may help you feel more relaxed if you are feeling anxious or panicky.
Breathing from the tummy does not come naturally. You should practice it when you are not breathless. This will help you learn the technique.
Practicing tummy breathing
- Find a comfortable position with your head and back supported, and your shoulders and upper chest relaxed.
- Place one hand on your tummy.
- Feel your tummy rise and expand as you breathe in and relax down as you breathe out.
- Breathe gently when practising - there should only be a slight movement of your tummy at rest.
Coronavirus recovery help - practicing tummy breathing
Breathe low and slow
Taking slower, deeper breaths from your tummy helps to ease shortness of breath.
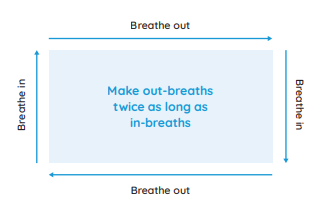
Breathe a rectangle
When you practice relaxed tummy breathing, it might help to picture a rectangle. This could be a book, a TV, window, table top, or a picture on the wall.
Pursed lip breathing
Pursed lip breathing can help if you:
- are very short of breath
- feel anxious
- find tummy breathing difficult
When you do pursed lip breathing, it takes more time for the air to leave your lungs. This makes it easier to take the next breath in.
- Breathe in through your nose.
- Purse your lips and breathe out.
- Continue until you feel your breathing is under control - think of it as blowing away your shortness of breath.
Managing shortness of breath
You can have shortness of breath even if your initial illness was mild. Many people feel better in a few days or weeks after a COVID-19 infection has gone. Most people will make a full recovery within 12 weeks.
But for some people, symptoms can last longer. COVID-19 usually affects the respiratory system. This can sometimes cause a lung injury that can take time to recover.
When you do everyday tasks and physical activity, take regular breaks and stop before you get too short of breath. You should be able to have a conversation while you do everyday tasks.
Pacing your activities over the day or week can help.
How to plan, prioritise and pace your activities as you recover
Progress may feel slow but be patient with yourself.
Increase your activities at your own pace when you:
- can maintain a level of activity without getting symptoms
- are confident you can do a bit more
Increasing your activity levels
When to get medical help
Most people can manage shortness of breath at home as they recover. But sometimes shortness of breath can be serious and you'll need to get medical help.
Emergency action required: Call 112 or 999 if:
- your chest feels tight or heavy
- you have pain that spreads to your arms, back, neck and jaw
- you suddenly feel or are being sick and have problems breathing
You could be having a heart attack or a problem with your lungs or airway.
Non-urgent advice: Phone your GP if
you have shortness of breath and:
- it does not improve or gets worse
- your breathing changes from what is normal or you are worried
- it gets worse when you have been active or when you lie down
- you have been coughing for 3 weeks or more
- you have swollen ankles
Quit smoking
If you smoke and have shortness of breath, you should quit smoking.
We provide free support to smokers who are thinking of quitting. This support is available on the phone, online or in person.
Content contributed by the Irish Society of Chartered Physiotherapists